Main Article Content
Abstract
Background: Globally, maternal mortality has remained unacceptably high with postpartum hemorrhage as the leading cause of maternal deaths All mothers are at risk of postpartum hemorrhage but there are predisposing influences that increase the risk of the mothers having postpartum hemorrhage or dying from it.
Objectives: The aim was to investigate the predisposing influences to postpartum hemorrhage in Mbarara and establish health facility readiness.
Methods: In this descriptive cross-sectional study that was quantitative in nature, 88 mothers attending postnatal care clinic at six weeks and had experienced postpartum hemorrhage in their recent childbirth were enrolled from six Health facilities. Researcher administered questionnaire was used to collect quantitative data.
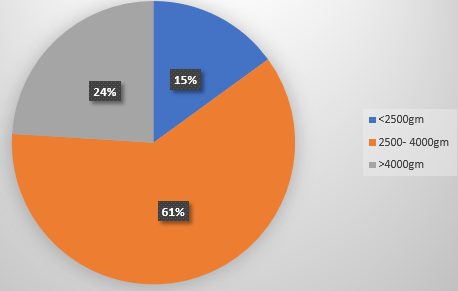
Results: Majority of the mothers,71 (80.7%) were aged 20-34 years; 69 (78.4%) had attended antenatal care clinic more than four times. The obstetric factor predisposing mothers to postpartum hemorrhage were mainly prolonged labour 57 (64.8%) and multiparous without caesarian section were 41 (46.6%). Only 50%of health facilities assessed were ready to manage postpartum hemorrhage.
Conclusion: The majority of the mothers who experienced postpartum hemorrhage had prolonged labour which could be explained by the three-delay model. Therefore, Health workers need to work continually to ensure that delays at all levels are reduced.
Keywords
Article Details
Copyright (c) 2023 Agatha Nshabohurira, Josephine Gbobbo, Tella Adedayo

This work is licensed under a Creative Commons Attribution 4.0 International License.
References
- Al-beity, F., Pembe, A. B., Kwezi, H. A., Massawe, S. N., Hanson, C., & Baker, U. (2020). “We do what we can do to save a woman” health workers’ perceptions of health facility readiness for management of postpartum haemorrhage.Global Health Action,13(1). https://doi.org/10.1080/16549716.2019.1707403.
- BazirBazirete O., Nzayirambaho, M., Umubyeyi, A., Uwimana, M. C., & Evans, M. (2020). Influencing factors for prevention of postpartum hemorrhage and early detection of childbearing women at risk in Northern Province of Rwanda: Beneficiary and health worker perspectives. BioMed Central Pregnancy and Childbirth, 20(1). https://doi.org/10.1186/s12884-020-03389-7
- Burwick, R. M., Newman, R. A., & Rincon, M. (2022). Mild anemia and risk of postpartum hemorrhage or blood transfusion in preeclampsia. American Journal of Obstetrics and Gynecology, 226(1), S281–S282. https://doi.org/10.1016/j.ajog.2021.11.478Corbetta-
- Rastelli, C. M., Friedman, A. M., Sobhani, N. C., Arditi, B., Goffman, D., & Wen, T. (2023). Postpartum hemorrhage trends and outcomes in the United States, 2000–2019.Obstetrics & Gynecology,141(1), 152-161.
- Davis, J., & Nelson, S. (n.d.). Association between breastfeeding, oxytocin, and risk of association between breastfeeding, oxytocin, and risk of postpartum hemorrhage postpartum hemorrhage. https://scholarworks.uark.edu/nursuht
- Dusingizimana, T., Ramilan, T., Weber, J. L., Iversen, P. O., Mugabowindekwe, M., Ahishakiye, J., & Brough, L. (2023). Predictors for achieving adequate antenatal care visits during pregnancy: A cross-sectional study in rural Northwest Rwanda. BioMed Central Pregnancy and Childbirth, 23(1). https://doi.org/10.1186/s12884-023-05384-0
- Gashaw Kettema, W., Tefera Ayele, Z., Assefaw Geremew, M., Temesgen Assefa, K., Ayalew Yimer, S., Dessie Liyew, A., Berihun Erega, B., & Habtie Dagnaw, E. (2023). Knowledge, utilization, and associated factors of nonpneumatic antishock garments for management of postpartum hemorrhage among maternity ward health care professionals in South Wollo Zone health facilities, Ethiopia, 2021: A cross-sectional study design. Obstetrics and Gynecology International, 2023. https://doi.org/10.1155/2023/8247603
- Habitamu, D., Goshu, Y. A., & Zeleke, L. B. (2019). The magnitude and associated factors of postpartum hemorrhage among mothers who delivered at Debre Tabor general hospital 2018. BioMed Central Research Notes, 12(1). https://doi.org/10.1186/s13104-019-4646-9
- Hamson, K., Ngonzi, J., Julius, M., Emmanuel, B., & Ronald, M. (2016). Prevalence, morphological types and factors associated with anemia among mothers attending antenatal clinic at Mbarara regional referral hospital, South Western Uganda.
- Li, N., Liu, Y., Yun, A., & Song, S. (2022). Correlation of Platelet Function with Postpartum Hemorrhage and Venous Thromboembolism in Patients with Gestational Hypertension Complicated with Diabetes.Computational and Mathematical Methods in Medicine, 22(1). https://doi.org/10.1155/2022/2423333
- Mahamoud, N. K., Mwambi, B., Oyet, C., Segujja, F., Webbo, F., Okiria, J. C., & Taremwa, I. M. (2020). Prevalence of anemia and its associated socio-demographic factors among pregnant women attending an antenatal care clinic at Kisugu Health Center IV, Makindye Division, Kampala, Uganda.Journal of blood medicine, 13-18.
- Marshal, J., Raynor, M. (2020). Myles textbook for midwives .Elsevier(INR).https://www.amazon.com/MYLES-TEXTBOOK-MIDWIVES-ACCESS-CODE/dp/0702076430
- Muhal, P., Kumar Gurjar, A., Sharma, G., Ashdhir, P., & Ashdhir Professor, P. (n.d.). Impact of postpartum hemorrhage in maternal near miss cases. European Journal of Molecular & Clinical Medicine, 9(8).
- Ngonzi, J., Mugyenyi, G., Kivunike, M., Mugisha, J., Salongo, W., Masembe, S., ... & Bajunirwe, F. (2019). Frequency of HIV status disclosure, associated factors and outcomes among HIV positive pregnant women at Mbarara Regional Referral Hospital, southwestern Uganda.Pan African Medical Journal,32(1).
- Ononge,S.,Mirembe,F.,Wandabwa,J.,Campbell. (2016) Incidence and risk factors for postpartum hemorrhage in Uganda.Reproductive Health13(38). https://doi.org/10.1186/s12978-016-0154-8.
- Nigu Nigussie, J., Girma, B., Molla, A., Tamir, T., & Tilahun, R. (2022). Magnitude of postpartum hemorrhage and its associated factors in Ethiopia: a systematic review and meta-analysis. Reproductive Health, 19(1). https://doi.org/10.1186/s12978-022-01360-7
- Tolossa, T., Fetensa, G., Zewde, E. A., Besho, M., & Jidha, T. D. (2022). Magnitude of postpartum hemorrhage and associated factors among women who gave birth in Ethiopia: A systematic review and meta-analysis. Reproductive Health. BioMed Central Limited,19(1) https://doi.org/10.1186/s12978-022-01498-4
- WHO, UNICEF,UNFPA,World Bank Group & the United Nations Population Division. (2019)WHO recommendations for the prevention and treatment of postpartum h emorrhage. (n.d.). www.who.int/maternal_child_adolescent
- Zenebe, G. A., Zenebe, W. A., Ewunie, T. M., & Dires, S. (2023). Primary postpartum hemorrhage and associated factors among delivering women in Gedeo Zone, Southern Ethiopia. Frontiers in Medicine, 10.https://doi.org/10.3389/fmed.2023.1096501.
References
Al-beity, F., Pembe, A. B., Kwezi, H. A., Massawe, S. N., Hanson, C., & Baker, U. (2020). “We do what we can do to save a woman” health workers’ perceptions of health facility readiness for management of postpartum haemorrhage.Global Health Action,13(1). https://doi.org/10.1080/16549716.2019.1707403.
BazirBazirete O., Nzayirambaho, M., Umubyeyi, A., Uwimana, M. C., & Evans, M. (2020). Influencing factors for prevention of postpartum hemorrhage and early detection of childbearing women at risk in Northern Province of Rwanda: Beneficiary and health worker perspectives. BioMed Central Pregnancy and Childbirth, 20(1). https://doi.org/10.1186/s12884-020-03389-7
Burwick, R. M., Newman, R. A., & Rincon, M. (2022). Mild anemia and risk of postpartum hemorrhage or blood transfusion in preeclampsia. American Journal of Obstetrics and Gynecology, 226(1), S281–S282. https://doi.org/10.1016/j.ajog.2021.11.478Corbetta-
Rastelli, C. M., Friedman, A. M., Sobhani, N. C., Arditi, B., Goffman, D., & Wen, T. (2023). Postpartum hemorrhage trends and outcomes in the United States, 2000–2019.Obstetrics & Gynecology,141(1), 152-161.
Davis, J., & Nelson, S. (n.d.). Association between breastfeeding, oxytocin, and risk of association between breastfeeding, oxytocin, and risk of postpartum hemorrhage postpartum hemorrhage. https://scholarworks.uark.edu/nursuht
Dusingizimana, T., Ramilan, T., Weber, J. L., Iversen, P. O., Mugabowindekwe, M., Ahishakiye, J., & Brough, L. (2023). Predictors for achieving adequate antenatal care visits during pregnancy: A cross-sectional study in rural Northwest Rwanda. BioMed Central Pregnancy and Childbirth, 23(1). https://doi.org/10.1186/s12884-023-05384-0
Gashaw Kettema, W., Tefera Ayele, Z., Assefaw Geremew, M., Temesgen Assefa, K., Ayalew Yimer, S., Dessie Liyew, A., Berihun Erega, B., & Habtie Dagnaw, E. (2023). Knowledge, utilization, and associated factors of nonpneumatic antishock garments for management of postpartum hemorrhage among maternity ward health care professionals in South Wollo Zone health facilities, Ethiopia, 2021: A cross-sectional study design. Obstetrics and Gynecology International, 2023. https://doi.org/10.1155/2023/8247603
Habitamu, D., Goshu, Y. A., & Zeleke, L. B. (2019). The magnitude and associated factors of postpartum hemorrhage among mothers who delivered at Debre Tabor general hospital 2018. BioMed Central Research Notes, 12(1). https://doi.org/10.1186/s13104-019-4646-9
Hamson, K., Ngonzi, J., Julius, M., Emmanuel, B., & Ronald, M. (2016). Prevalence, morphological types and factors associated with anemia among mothers attending antenatal clinic at Mbarara regional referral hospital, South Western Uganda.
Li, N., Liu, Y., Yun, A., & Song, S. (2022). Correlation of Platelet Function with Postpartum Hemorrhage and Venous Thromboembolism in Patients with Gestational Hypertension Complicated with Diabetes.Computational and Mathematical Methods in Medicine, 22(1). https://doi.org/10.1155/2022/2423333
Mahamoud, N. K., Mwambi, B., Oyet, C., Segujja, F., Webbo, F., Okiria, J. C., & Taremwa, I. M. (2020). Prevalence of anemia and its associated socio-demographic factors among pregnant women attending an antenatal care clinic at Kisugu Health Center IV, Makindye Division, Kampala, Uganda.Journal of blood medicine, 13-18.
Marshal, J., Raynor, M. (2020). Myles textbook for midwives .Elsevier(INR).https://www.amazon.com/MYLES-TEXTBOOK-MIDWIVES-ACCESS-CODE/dp/0702076430
Muhal, P., Kumar Gurjar, A., Sharma, G., Ashdhir, P., & Ashdhir Professor, P. (n.d.). Impact of postpartum hemorrhage in maternal near miss cases. European Journal of Molecular & Clinical Medicine, 9(8).
Ngonzi, J., Mugyenyi, G., Kivunike, M., Mugisha, J., Salongo, W., Masembe, S., ... & Bajunirwe, F. (2019). Frequency of HIV status disclosure, associated factors and outcomes among HIV positive pregnant women at Mbarara Regional Referral Hospital, southwestern Uganda.Pan African Medical Journal,32(1).
Ononge,S.,Mirembe,F.,Wandabwa,J.,Campbell. (2016) Incidence and risk factors for postpartum hemorrhage in Uganda.Reproductive Health13(38). https://doi.org/10.1186/s12978-016-0154-8.
Nigu Nigussie, J., Girma, B., Molla, A., Tamir, T., & Tilahun, R. (2022). Magnitude of postpartum hemorrhage and its associated factors in Ethiopia: a systematic review and meta-analysis. Reproductive Health, 19(1). https://doi.org/10.1186/s12978-022-01360-7
Tolossa, T., Fetensa, G., Zewde, E. A., Besho, M., & Jidha, T. D. (2022). Magnitude of postpartum hemorrhage and associated factors among women who gave birth in Ethiopia: A systematic review and meta-analysis. Reproductive Health. BioMed Central Limited,19(1) https://doi.org/10.1186/s12978-022-01498-4
WHO, UNICEF,UNFPA,World Bank Group & the United Nations Population Division. (2019)WHO recommendations for the prevention and treatment of postpartum h emorrhage. (n.d.). www.who.int/maternal_child_adolescent
Zenebe, G. A., Zenebe, W. A., Ewunie, T. M., & Dires, S. (2023). Primary postpartum hemorrhage and associated factors among delivering women in Gedeo Zone, Southern Ethiopia. Frontiers in Medicine, 10.https://doi.org/10.3389/fmed.2023.1096501.