Main Article Content
Abstract
Surgical site infections (SSIs) are a global healthcare challenge. The Pseudomonas aeruginosa is a significant SSI pathogen with the oprL gene conferring its multidrug resistance. Although extensive studies on pathogens in infection control are recommended, a study of this kind has not been conducted in Bauchi, Nigeria.
Objectives: This study determined the prevalence and associated factors for SSIs linked with P. aeruginosa with oprL gene. Surgical site swabs (n=250) collected from two hospitals in Bauchi, Nigeria, were cultured on Cetrimide agar to isolate P. aeruginosa. The oprL genes of the isolates were detected through a Polymerase chain Reaction. Chi-square tests, Fisher's exact test, and binary logistic regression analyzed the association between SSIs and other variables. About 2% (5/250) of the swabs were infected with P. aeruginosa with oprL gene. SSI occurrence was statistically associated with post-operative duration (p = 0.01). Prolonged postoperative periods increased the odds of developing SSIs by a factor of 3.81 (O.R.:3.81, p=0.02). No significant associations were found between SSIs and sex (p = 0.65), age (p = 0.09), surgery (p = 0.06), and HIV status (p = 0.31). The prevalence of P. aeruginosa linked to SSIs was low. Prolonged postoperative care significantly increased the risk of SSIs. Future research with longitudinal designs and large samples will monitor additional risk factors of SSIs. Infection control should emphasize post-operative care for SSIs.The integration of molecular confirmation of P. aeruginosa isolates should be routine in SSI management.
Keywords
Article Details

This work is licensed under a Creative Commons Attribution 4.0 International License.
References
- Abiodun, A., Ogunjobi, A. A., & Oluwatosin, O. M. (2014). Multidrug resistance and virulence genes in Escherichia coli and Pseudomonas aeruginosa isolated from diabetic foot infections. African Journal of Clinical and Experimental Microbiology, 15(2), 64-72.
- Adhikari, S., Khadka, S., Sapkota, S., et al. (2019). Prevalence and antibiograms of uropathogens from the suspected cases of urinary tract infections in Bharatpur Hospital, Nepal. Journal of College of Medical Sciences-Nepal, 15(4), 260-266.
- Anuj, S. N., Whiley, D. M., Kidd, T. J., Bell, S. C., Wainwright, C. E., Nissen, M. D., & Sloots, T. P. (2009). Identification of Pseudomonas aeruginosa by a duplex real-time polymerase chain reaction assay targeting the ecfX and the gyrB genes. Diagnostic Microbiology and Infectious Disease, 63, 127-131.
- Bartholomew, J. W., & Mittwer, T. (1952). The gram stain. Bacteriological reviews, 16(1), 1-29.
- Berríos-Torres, S. I. (2017). Centers for Disease Control and Prevention Guideline for the Prevention of Surgical Site Infection. JAMA Surgery, 152(8), 784.
- Brandenburg, K. S., Calderon, D. F., Kierski, P. R., Brown, A. L., Shah, N. M., Abbott, N. L., ... & Czuprynski, C. J. (2015). Inhibition of Pseudomonas aeruginosa biofilm formation on wound dressings. Wound Repair and Regeneration, 23(6), 842-854. https://doi.org/10.1111/wrr.12365
- Bucataru, A., Balasoiu, M., Ghenea, A. E., Zlatian, O. M., Vulcanescu, D. D., Horhat, F. G., ... & Mogoanta, S. S. (2023). Factors contributing to surgical site infections: A comprehensive systematic review of etiology and risk factors. Clin Pract, 14(1), 52-68. https://doi.org/10.3390/clinpract14010006
- Choi, J. Y., Sifri, C. D., Goumnerov, B. C., Rahme, L. G., Ausubel, F. M., & Calderwood, S. B. (2002). Identification of virulence genes in a pathogenic strain of Pseudomonas aeruginosa by representational difference analysis. Journal of Bacteriology, 184(4), 952-961. https://doi.org/10.1128/JB.184.4.952-961.2002
- Cochran, W. G. (1963). Sampling techniques (2nd ed.). New York: John Wiley and Sons Inc.
- dela Merced, P. A., Nadler, E. P., & Hamdy, R. F. (2021). Surgical site infections (SSI) – Prophylaxis and management. In S. T. Verghese & T. D. Kane (Eds.), Anesthetic management in pediatric general surgery. Springer, Cham. https://doi.org/10.1007/978-3-030-72551-8_7
- Deschaght, P., Van Daele, S., De Baets, F., & Vaneechoutte, M. (2011). PCR and the detection of Pseudomonas aeruginosa in respiratory samples of CF patients: A literature review. Journal of Cystic Fibrosis, 10(5), 293-297. https://doi.org/10.1016/j.jcf.2011.05.004
- El Zowalaty, M. E., & Gyetvai, B. (2016). Effectiveness of Antipseudomonal Antibiotics and Mechanisms of Multidrug Resistance in Pseudomonas aeruginosa. Polish Journal of Microbiology, 65(1), 23-32.
- Galloway, D. R. (1991). Pseudomonas aeruginosa elastase and elastolysis revisited: Recent developments. Molecular Microbiology, 5(10), 2315-2321. https://doi.org/10.1111/j.1365-2958.1991.tb02076.x
- Garcia, M., Morello, E., Garnier, J., Barrault, C., Garnier, M., & Burucoa, C. (2018). Pseudomonas aeruginosa flagellum is critical for invasion, cutaneous persistence and induction of inflammatory response of skin epidermis. Virulence, 9(1), 1163-1175. https://doi.org/10.1080/21505594.2018.1480830
- Haghi, F., Zeighami, H., Monazami, A., Toutouchi, F., Nazaralian, S., & Naderi, G. (2018). Diversity of virulence genes in multidrug-resistant Pseudomonas aeruginosa isolated from burn wound infections. Microbial Pathogenesis, 115, 251-256. https://doi.org/10.1016/j.micpath.2017.12.052
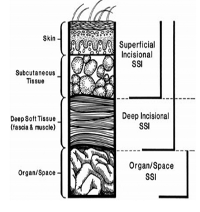
- Horan, T. C., Gaynes, R. P., Martone, W. J., Jarvis, W. R., & Emori, T. G. (1992). CDC definitions of nosocomial surgical site infections, 1992: A modification of CDC definitions of surgical wound infections. Infection Control & Hospital Epidemiology, 13(10), 606-608.
- Jensen, L. K., Johansen, A. S. B., & Jensen, H. E. (2017). Porcine models of biofilm infections with focus on pathomorphology. Frontiers in Microbiology, 8, 1961. https://doi.org/10.3389/fmicb.2017.01961
- Kaplan, N., Smadi, A., Al-Taani, M., & El-Qudah, M. (2003). Microbiology of wound infection after cesarean section in a Jordanian hospital. East Mediterr Health J., 9(5/6), 1069-1075.
- Kaye, K. S., Pogue, J. M., Tran, T. B., Nation, R. L., & Li, J. (2019). Agents of last resort: Polymyxin resistance. Infectious Disease Clinics of North America, 33(4), 835-851. https://doi.org/10.1016/j.idc.2019.08.010
- Klockgether, J., & Tümmler, B. (2017). Recent advances in understanding Pseudomonas aeruginosa as a pathogen. F1000Research, 6, 1261. https://doi.org/10.12688/f1000research.10506.1
- Lamichhane, A., Sapkota, S., Khadka, S., et al. (2020). Incidence of ESBL-producing Gram-negative bacteria of lower respiratory tract infection in Bharatpur Hospital, Nepal. Anti-Infective Agents, 18.
- Lee, J., & Zhang, L. (2015). The hierarchy quorum sensing network in Pseudomonas aeruginosa. Protein & Cell, 6, 26-41. https://doi.org/10.1007/s13238-014-0100-x
- Mann, C. J. (2003). Observational research methods. Research design II: Cohort, cross-sectional and case-control studies. Emerg Med J., 20(1), 54-60. https://doi.org/10.1136/emj.20.1.54
- Marzoug, O. A., Anees, A., & Malik, E. M. (2023). Assessment of risk factors associated with surgical site infection following abdominal surgery: A systematic review. BMJ Surgery, Interventions, & Health Technologies, 5(1), e000182. https://doi.org/10.1136/bmjsit-2023-000182
- Maunders, E., & Welch, M. (2017). Matrix exopolysaccharides; the sticky side of biofilm formation. FEMS Microbiology Letters, 364(15). https://doi.org/10.1093/femsle/fnx120
- McKnight, S. L., Iglewski, B. H., & Pesci, E. C. (2000). The Pseudomonas quinolone signal regulates rhl quorum sensing in Pseudomonas aeruginosa. Journal of Bacteriology, 182(10), 2702-2708. https://doi.org/10.1128/JB.182.10.2702-2708.2000
- Mohammad, H. H. (2013). Phenotypic Investigation for Virulence Factors of Pyocine Producing Pseudomonas aeruginosa Isolated from Burn Wounds, Iraq. International Journal of Scientific & Engineering Research, 4(7), 2114-2121.
- Monk, E. J. M., Jones, T. P. W., Bongomin, F., Kibone, W., Nsubuga, Y., Ssewante, N., Muleya, I., Nsenga, L., Rao, V. B., & van Zandvoort, K. (2024). Antimicrobial resistance in bacterial wound, skin, soft tissue, and surgical site infections in Central, Eastern, Southern, and Western Africa: A systematic review and meta-analysis.PLOS Global Public Health, 4(4), e0003077. https://doi.org/10.1371/journal.pgph.0003077
- Nguyen, T., Kaye, K. S., & Ho, D. (2020). Comprehensive data collection for accurate risk assessment in SSIs. American Journal of Infection Control, 48(6), 669-675. https://doi.org/10.1016/j.ajic.2020.01.017
- Olowo-Okere, A., Ibrahim, Y., Olayinka, B. O., & Ehinmidu, J. O. (2019). Epidemiology of surgical site infections in Nigeria: A systematic review and meta-analysis. The Nigerian Postgraduate Medical Journal, 26(3), 143-151. https://doi.org/10.4103/npmj.npmj_72_
- Onuh, C. O. (2019). Site location map: Shadowanka and Bayara areas of Bauchi, Nigeria.
- Onyi, T., Doko, H., & Ella, E. (2024). Molecular detection of oprL gene in Pseudomonas aeruginosa associated with surgical site infections in Bauchi, Nigeria. Microbes and Infectious Diseases. https://doi.org/10.21608/mid.2024.261508.1750
- Onyi, T., Doko, H., & Ella, E. (2024). The antibiogram of multidrug-resistant Pseudomonas aeruginosa with oprL gene associated with surgical site infections in Bauchi, Nigeria. Microbes and Infectious Diseases. https://doi.org/10.21608/mid.2024.261574.1752
- Paul, J. P. (2018). Pseudomonas aeruginosa. In Principles and Practice of Pediatric Infectious Diseases (pp. 866-870.e1).
- Penn State University. (n.d.). Lesson 8 - Bias, confounding, random error, and effect modification. Retrieved from https://online.stat.psu.edu/stat507/book/export/html/762
- Peters, J. E., & Galloway, D. R. (1990). Purification and characterization of an active fragment of the LasA protein from Pseudomonas aeruginosa: enhancement of elastase activity. Journal of Bacteriology, 172(5), 2236-2240. https://doi.org/10.1128/jb.172.5.2236-2240.1990
- Pinchera, B., Buonomo, A. R., Schiano Moriello, N., Scotto, R., Villari, R., & Gentile, I. (2022). Update on the management of surgical site infections. Antibiotics, 11, 1608.
- Pollack, M. (2000). Pseudomonas aeruginosa. In G. L. Mandell, J. E. Bennett, & R. Dolin (Eds.), Principles and Practice of Infectious Diseases (5th ed., pp. 2310-2327). Churchill Livingstone.
- Public Health England. (2015). Identification of Pseudomonas species and other Non-Glucose Fermenters. UK Standards for Microbiology Investigations, ID 17, Issue 3. Retrieved from [https://www.gov.uk/uk-standards-for-microbiology-investigations-smi-quality-and-consistency-in-clinical-laboratories](https://www.gov.uk/uk-standards-for-microbiology-investigations-smi-quality-and-consistency-in-clinical-laboratories).
- Reid, T. M., & Porter, I. A. (1981). An outbreak of otitis externa in competitive swimmers due to Pseudomonas aeruginosa. Journal of Hygiene, 86(3), 357-362. https://doi.org/10.1017/s0022172400069114
- Rogers, B. A., Sidjabat, H. E., & Paterson, D. L. (2018). Escherichia coli O25b-ST131: A pandemic multiresistant community-associated strain. The Journal of Antimicrobial Chemotherapy, 73(1), 173-181. https://doi.org/10.1093/jac/dkx430
- Shah, S., Singhal, T., Naik, R., & Thakkar, P. (2020). Predominance of Multidrug-Resistant Gram-Negative Organisms as Cause of Surgical Site Infections at a Private Tertiary Care Hospital in Mumbai, India. Indian Journal of Medical Microbiology, 38, 344–350
- Tacconelli, E., Carrara, E., Savoldi, A., Harbarth, S., Mendelson, M., Monnet, D. L., ... & the WHO Pathogens Priority List Working Group. (2018). Discovery, research, and development of new antibiotics: The WHO priority list of antibiotic-resistant bacteria and tuberculosis. Lancet Infectious Diseases, 18, 318-327. https://doi.org/10.1016/S1473-3099(17)30753-3
- Tang, Y., Ali, Z., Zou, J., Jin, G., Zhu, J., Yang, J., & Dai, J. (2017). Detection methods for Pseudomonas aeruginosa: history and future perspective. RSC Advances, 7, 51789-51800. https://doi.org/10.1039/c7ra09064a
- Tornero, E., Morata, L., Martínez-Pastor, J. C., Angulo, S., Combalia, A., Bori, G., & Soriano, A. (2018). Prosthetic joint infection due to Pseudomonas aeruginosa: Outcome of a difficult-to-treat infection with limited treatment options. Journal of Clinical Medicine, 7(3), 67.
- Tuon, F. F., Cieslinski, J., Ono, A. F. M., Goto, F. L., Machinski, J. M., Mantovani, L. K., Kosop, L. R., Namba, M. S., & Rocha, J. L. (2019). Microbiological profile and susceptibility pattern of surgical site infections related to orthopaedic trauma. International Orthopaedics, 43(6), 1309-1313. https://doi.org/10.1007/s00264-018-4076-7
- World Health Organization. (2017). Prioritization of pathogens to guide discovery, research and development of new antibiotics for drug-resistant bacterial infections including tuberculosis. Geneva: World Health Organization. (WHO/EMP/IAU/2017.12).
- World Health Organization. (2018). Infection control. Retrieved from https://apps.who.int/iris/bitstream/handle/10665/277399/9789241550475-eng.pdf?ua=1.
- Wu, W., Jin, Y., Bai, F., & Jin, S. (2015). Pseudomonas aeruginosa. In Molecular Medical Microbiology (pp. 753-767). Elsevier.
- Xu, Y., Chen, W., You, C., & Liu, Z. (2017). Development of a multiplex PCR assay for detection of Pseudomonas fluorescens with biofilm formation ability. Journal of Food Science, 82(10), 2337-2342. https://doi.org/10.1111/1750-3841.13845
- Yasidi, B. M., Denue, B. A., Onah, J. O., Jibrin, Y. B., Umar, H. M., Gabchiya, N. M., ... & Okon, K. O. (2015). Retrospective analysis of bacterial pathogens isolated from wound infections at a tertiary hospital in Nguru, Yobe State, Nigeria. American Journal of Biomedical and Life Sciences, 3(1), 1-6. https://doi.org/10.11648/j.asjbls.20150301.11
References
Abiodun, A., Ogunjobi, A. A., & Oluwatosin, O. M. (2014). Multidrug resistance and virulence genes in Escherichia coli and Pseudomonas aeruginosa isolated from diabetic foot infections. African Journal of Clinical and Experimental Microbiology, 15(2), 64-72.
Adhikari, S., Khadka, S., Sapkota, S., et al. (2019). Prevalence and antibiograms of uropathogens from the suspected cases of urinary tract infections in Bharatpur Hospital, Nepal. Journal of College of Medical Sciences-Nepal, 15(4), 260-266.
Anuj, S. N., Whiley, D. M., Kidd, T. J., Bell, S. C., Wainwright, C. E., Nissen, M. D., & Sloots, T. P. (2009). Identification of Pseudomonas aeruginosa by a duplex real-time polymerase chain reaction assay targeting the ecfX and the gyrB genes. Diagnostic Microbiology and Infectious Disease, 63, 127-131.
Bartholomew, J. W., & Mittwer, T. (1952). The gram stain. Bacteriological reviews, 16(1), 1-29.
Berríos-Torres, S. I. (2017). Centers for Disease Control and Prevention Guideline for the Prevention of Surgical Site Infection. JAMA Surgery, 152(8), 784.
Brandenburg, K. S., Calderon, D. F., Kierski, P. R., Brown, A. L., Shah, N. M., Abbott, N. L., ... & Czuprynski, C. J. (2015). Inhibition of Pseudomonas aeruginosa biofilm formation on wound dressings. Wound Repair and Regeneration, 23(6), 842-854. https://doi.org/10.1111/wrr.12365
Bucataru, A., Balasoiu, M., Ghenea, A. E., Zlatian, O. M., Vulcanescu, D. D., Horhat, F. G., ... & Mogoanta, S. S. (2023). Factors contributing to surgical site infections: A comprehensive systematic review of etiology and risk factors. Clin Pract, 14(1), 52-68. https://doi.org/10.3390/clinpract14010006
Choi, J. Y., Sifri, C. D., Goumnerov, B. C., Rahme, L. G., Ausubel, F. M., & Calderwood, S. B. (2002). Identification of virulence genes in a pathogenic strain of Pseudomonas aeruginosa by representational difference analysis. Journal of Bacteriology, 184(4), 952-961. https://doi.org/10.1128/JB.184.4.952-961.2002
Cochran, W. G. (1963). Sampling techniques (2nd ed.). New York: John Wiley and Sons Inc.
dela Merced, P. A., Nadler, E. P., & Hamdy, R. F. (2021). Surgical site infections (SSI) – Prophylaxis and management. In S. T. Verghese & T. D. Kane (Eds.), Anesthetic management in pediatric general surgery. Springer, Cham. https://doi.org/10.1007/978-3-030-72551-8_7
Deschaght, P., Van Daele, S., De Baets, F., & Vaneechoutte, M. (2011). PCR and the detection of Pseudomonas aeruginosa in respiratory samples of CF patients: A literature review. Journal of Cystic Fibrosis, 10(5), 293-297. https://doi.org/10.1016/j.jcf.2011.05.004
El Zowalaty, M. E., & Gyetvai, B. (2016). Effectiveness of Antipseudomonal Antibiotics and Mechanisms of Multidrug Resistance in Pseudomonas aeruginosa. Polish Journal of Microbiology, 65(1), 23-32.
Galloway, D. R. (1991). Pseudomonas aeruginosa elastase and elastolysis revisited: Recent developments. Molecular Microbiology, 5(10), 2315-2321. https://doi.org/10.1111/j.1365-2958.1991.tb02076.x
Garcia, M., Morello, E., Garnier, J., Barrault, C., Garnier, M., & Burucoa, C. (2018). Pseudomonas aeruginosa flagellum is critical for invasion, cutaneous persistence and induction of inflammatory response of skin epidermis. Virulence, 9(1), 1163-1175. https://doi.org/10.1080/21505594.2018.1480830
Haghi, F., Zeighami, H., Monazami, A., Toutouchi, F., Nazaralian, S., & Naderi, G. (2018). Diversity of virulence genes in multidrug-resistant Pseudomonas aeruginosa isolated from burn wound infections. Microbial Pathogenesis, 115, 251-256. https://doi.org/10.1016/j.micpath.2017.12.052
Horan, T. C., Gaynes, R. P., Martone, W. J., Jarvis, W. R., & Emori, T. G. (1992). CDC definitions of nosocomial surgical site infections, 1992: A modification of CDC definitions of surgical wound infections. Infection Control & Hospital Epidemiology, 13(10), 606-608.
Jensen, L. K., Johansen, A. S. B., & Jensen, H. E. (2017). Porcine models of biofilm infections with focus on pathomorphology. Frontiers in Microbiology, 8, 1961. https://doi.org/10.3389/fmicb.2017.01961
Kaplan, N., Smadi, A., Al-Taani, M., & El-Qudah, M. (2003). Microbiology of wound infection after cesarean section in a Jordanian hospital. East Mediterr Health J., 9(5/6), 1069-1075.
Kaye, K. S., Pogue, J. M., Tran, T. B., Nation, R. L., & Li, J. (2019). Agents of last resort: Polymyxin resistance. Infectious Disease Clinics of North America, 33(4), 835-851. https://doi.org/10.1016/j.idc.2019.08.010
Klockgether, J., & Tümmler, B. (2017). Recent advances in understanding Pseudomonas aeruginosa as a pathogen. F1000Research, 6, 1261. https://doi.org/10.12688/f1000research.10506.1
Lamichhane, A., Sapkota, S., Khadka, S., et al. (2020). Incidence of ESBL-producing Gram-negative bacteria of lower respiratory tract infection in Bharatpur Hospital, Nepal. Anti-Infective Agents, 18.
Lee, J., & Zhang, L. (2015). The hierarchy quorum sensing network in Pseudomonas aeruginosa. Protein & Cell, 6, 26-41. https://doi.org/10.1007/s13238-014-0100-x
Mann, C. J. (2003). Observational research methods. Research design II: Cohort, cross-sectional and case-control studies. Emerg Med J., 20(1), 54-60. https://doi.org/10.1136/emj.20.1.54
Marzoug, O. A., Anees, A., & Malik, E. M. (2023). Assessment of risk factors associated with surgical site infection following abdominal surgery: A systematic review. BMJ Surgery, Interventions, & Health Technologies, 5(1), e000182. https://doi.org/10.1136/bmjsit-2023-000182
Maunders, E., & Welch, M. (2017). Matrix exopolysaccharides; the sticky side of biofilm formation. FEMS Microbiology Letters, 364(15). https://doi.org/10.1093/femsle/fnx120
McKnight, S. L., Iglewski, B. H., & Pesci, E. C. (2000). The Pseudomonas quinolone signal regulates rhl quorum sensing in Pseudomonas aeruginosa. Journal of Bacteriology, 182(10), 2702-2708. https://doi.org/10.1128/JB.182.10.2702-2708.2000
Mohammad, H. H. (2013). Phenotypic Investigation for Virulence Factors of Pyocine Producing Pseudomonas aeruginosa Isolated from Burn Wounds, Iraq. International Journal of Scientific & Engineering Research, 4(7), 2114-2121.
Monk, E. J. M., Jones, T. P. W., Bongomin, F., Kibone, W., Nsubuga, Y., Ssewante, N., Muleya, I., Nsenga, L., Rao, V. B., & van Zandvoort, K. (2024). Antimicrobial resistance in bacterial wound, skin, soft tissue, and surgical site infections in Central, Eastern, Southern, and Western Africa: A systematic review and meta-analysis.PLOS Global Public Health, 4(4), e0003077. https://doi.org/10.1371/journal.pgph.0003077
Nguyen, T., Kaye, K. S., & Ho, D. (2020). Comprehensive data collection for accurate risk assessment in SSIs. American Journal of Infection Control, 48(6), 669-675. https://doi.org/10.1016/j.ajic.2020.01.017
Olowo-Okere, A., Ibrahim, Y., Olayinka, B. O., & Ehinmidu, J. O. (2019). Epidemiology of surgical site infections in Nigeria: A systematic review and meta-analysis. The Nigerian Postgraduate Medical Journal, 26(3), 143-151. https://doi.org/10.4103/npmj.npmj_72_
Onuh, C. O. (2019). Site location map: Shadowanka and Bayara areas of Bauchi, Nigeria.
Onyi, T., Doko, H., & Ella, E. (2024). Molecular detection of oprL gene in Pseudomonas aeruginosa associated with surgical site infections in Bauchi, Nigeria. Microbes and Infectious Diseases. https://doi.org/10.21608/mid.2024.261508.1750
Onyi, T., Doko, H., & Ella, E. (2024). The antibiogram of multidrug-resistant Pseudomonas aeruginosa with oprL gene associated with surgical site infections in Bauchi, Nigeria. Microbes and Infectious Diseases. https://doi.org/10.21608/mid.2024.261574.1752
Paul, J. P. (2018). Pseudomonas aeruginosa. In Principles and Practice of Pediatric Infectious Diseases (pp. 866-870.e1).
Penn State University. (n.d.). Lesson 8 - Bias, confounding, random error, and effect modification. Retrieved from https://online.stat.psu.edu/stat507/book/export/html/762
Peters, J. E., & Galloway, D. R. (1990). Purification and characterization of an active fragment of the LasA protein from Pseudomonas aeruginosa: enhancement of elastase activity. Journal of Bacteriology, 172(5), 2236-2240. https://doi.org/10.1128/jb.172.5.2236-2240.1990
Pinchera, B., Buonomo, A. R., Schiano Moriello, N., Scotto, R., Villari, R., & Gentile, I. (2022). Update on the management of surgical site infections. Antibiotics, 11, 1608.
Pollack, M. (2000). Pseudomonas aeruginosa. In G. L. Mandell, J. E. Bennett, & R. Dolin (Eds.), Principles and Practice of Infectious Diseases (5th ed., pp. 2310-2327). Churchill Livingstone.
Public Health England. (2015). Identification of Pseudomonas species and other Non-Glucose Fermenters. UK Standards for Microbiology Investigations, ID 17, Issue 3. Retrieved from [https://www.gov.uk/uk-standards-for-microbiology-investigations-smi-quality-and-consistency-in-clinical-laboratories](https://www.gov.uk/uk-standards-for-microbiology-investigations-smi-quality-and-consistency-in-clinical-laboratories).
Reid, T. M., & Porter, I. A. (1981). An outbreak of otitis externa in competitive swimmers due to Pseudomonas aeruginosa. Journal of Hygiene, 86(3), 357-362. https://doi.org/10.1017/s0022172400069114
Rogers, B. A., Sidjabat, H. E., & Paterson, D. L. (2018). Escherichia coli O25b-ST131: A pandemic multiresistant community-associated strain. The Journal of Antimicrobial Chemotherapy, 73(1), 173-181. https://doi.org/10.1093/jac/dkx430
Shah, S., Singhal, T., Naik, R., & Thakkar, P. (2020). Predominance of Multidrug-Resistant Gram-Negative Organisms as Cause of Surgical Site Infections at a Private Tertiary Care Hospital in Mumbai, India. Indian Journal of Medical Microbiology, 38, 344–350
Tacconelli, E., Carrara, E., Savoldi, A., Harbarth, S., Mendelson, M., Monnet, D. L., ... & the WHO Pathogens Priority List Working Group. (2018). Discovery, research, and development of new antibiotics: The WHO priority list of antibiotic-resistant bacteria and tuberculosis. Lancet Infectious Diseases, 18, 318-327. https://doi.org/10.1016/S1473-3099(17)30753-3
Tang, Y., Ali, Z., Zou, J., Jin, G., Zhu, J., Yang, J., & Dai, J. (2017). Detection methods for Pseudomonas aeruginosa: history and future perspective. RSC Advances, 7, 51789-51800. https://doi.org/10.1039/c7ra09064a
Tornero, E., Morata, L., Martínez-Pastor, J. C., Angulo, S., Combalia, A., Bori, G., & Soriano, A. (2018). Prosthetic joint infection due to Pseudomonas aeruginosa: Outcome of a difficult-to-treat infection with limited treatment options. Journal of Clinical Medicine, 7(3), 67.
Tuon, F. F., Cieslinski, J., Ono, A. F. M., Goto, F. L., Machinski, J. M., Mantovani, L. K., Kosop, L. R., Namba, M. S., & Rocha, J. L. (2019). Microbiological profile and susceptibility pattern of surgical site infections related to orthopaedic trauma. International Orthopaedics, 43(6), 1309-1313. https://doi.org/10.1007/s00264-018-4076-7
World Health Organization. (2017). Prioritization of pathogens to guide discovery, research and development of new antibiotics for drug-resistant bacterial infections including tuberculosis. Geneva: World Health Organization. (WHO/EMP/IAU/2017.12).
World Health Organization. (2018). Infection control. Retrieved from https://apps.who.int/iris/bitstream/handle/10665/277399/9789241550475-eng.pdf?ua=1.
Wu, W., Jin, Y., Bai, F., & Jin, S. (2015). Pseudomonas aeruginosa. In Molecular Medical Microbiology (pp. 753-767). Elsevier.
Xu, Y., Chen, W., You, C., & Liu, Z. (2017). Development of a multiplex PCR assay for detection of Pseudomonas fluorescens with biofilm formation ability. Journal of Food Science, 82(10), 2337-2342. https://doi.org/10.1111/1750-3841.13845
Yasidi, B. M., Denue, B. A., Onah, J. O., Jibrin, Y. B., Umar, H. M., Gabchiya, N. M., ... & Okon, K. O. (2015). Retrospective analysis of bacterial pathogens isolated from wound infections at a tertiary hospital in Nguru, Yobe State, Nigeria. American Journal of Biomedical and Life Sciences, 3(1), 1-6. https://doi.org/10.11648/j.asjbls.20150301.11